So I read this article in the ABC today titled, “Difficult people can be highly destructive. Psychologist Rebecca Ray has tips for dealing with them” and I had thoughts, specifically about this bit:
At work, psychological safety means having the freedom “to innovate, be creative, make mistakes and speak up with your ideas without fear of being shamed, humiliated or punished”, explains Dr Ray, the author of a new book called Difficult People.
That idea can be applied to other relationships, too. In all interactions, we should be able “to show up as our authentic selves, to be able to be imperfect, and to be able to connect vulnerably”, Dr Ray says.
My first thoughts were about the number of psychologically unsafe workplaces I’ve worked in over the past 15 years (thankfully not my current one) and how creativity was stifled, mistakes were punished, and vulnerability was attacked. I also thought about how I survived those workplaces when others struggled to.
When I was 13, my family moved from Alice Springs in the Northern Territory/Central Australia to Bendigo in Central Victoria. We went from a town of 30,000 at peak tourist season to a town of 75,000 at least, all the time (population now over 120,000). I went from a school of 250 people from year 7 to 10, to a school where there was 300 in one year level – so the junior campus (years 7 – 9) had 900 students.
I went from a town where I fit and my weirdness was accepted to a town where I was an outsider and my weirdness wasn’t tolerated. Suffice to say, Bendigo and the school I went to were incredibly psychologically unsafe and the cause of a part of my childhood trauma. I definitely wasn’t able to show up as my authentic self, and was regularly shamed, humiliated and punished. Things at home were also not great at the time, so it was a shit sandwich.
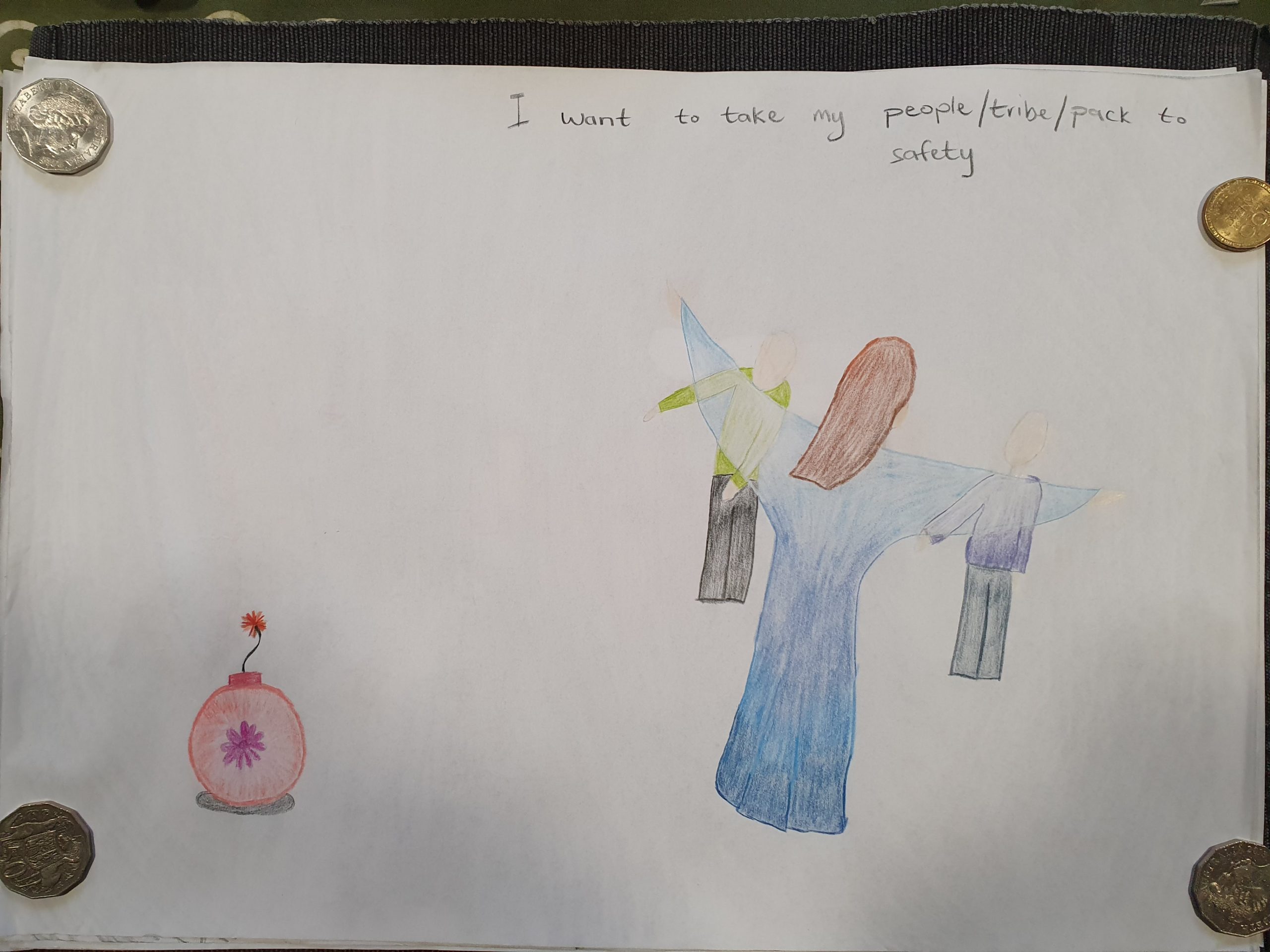
When I went to university (briefly) after year 12, I found my people. I was also in a very abusive relationship at the time and the people I found provided some shelter and a reality check to that relationship. My people collectively showed me I didn’t have to put up with psychological danger, that I could just be myself and let everyone else tie themselves in knots. I left that relationship, left Bendigo, left the university degree that I was never going to get (well not that one) and moved to Melbourne with a new relationship that was so much more healthier.
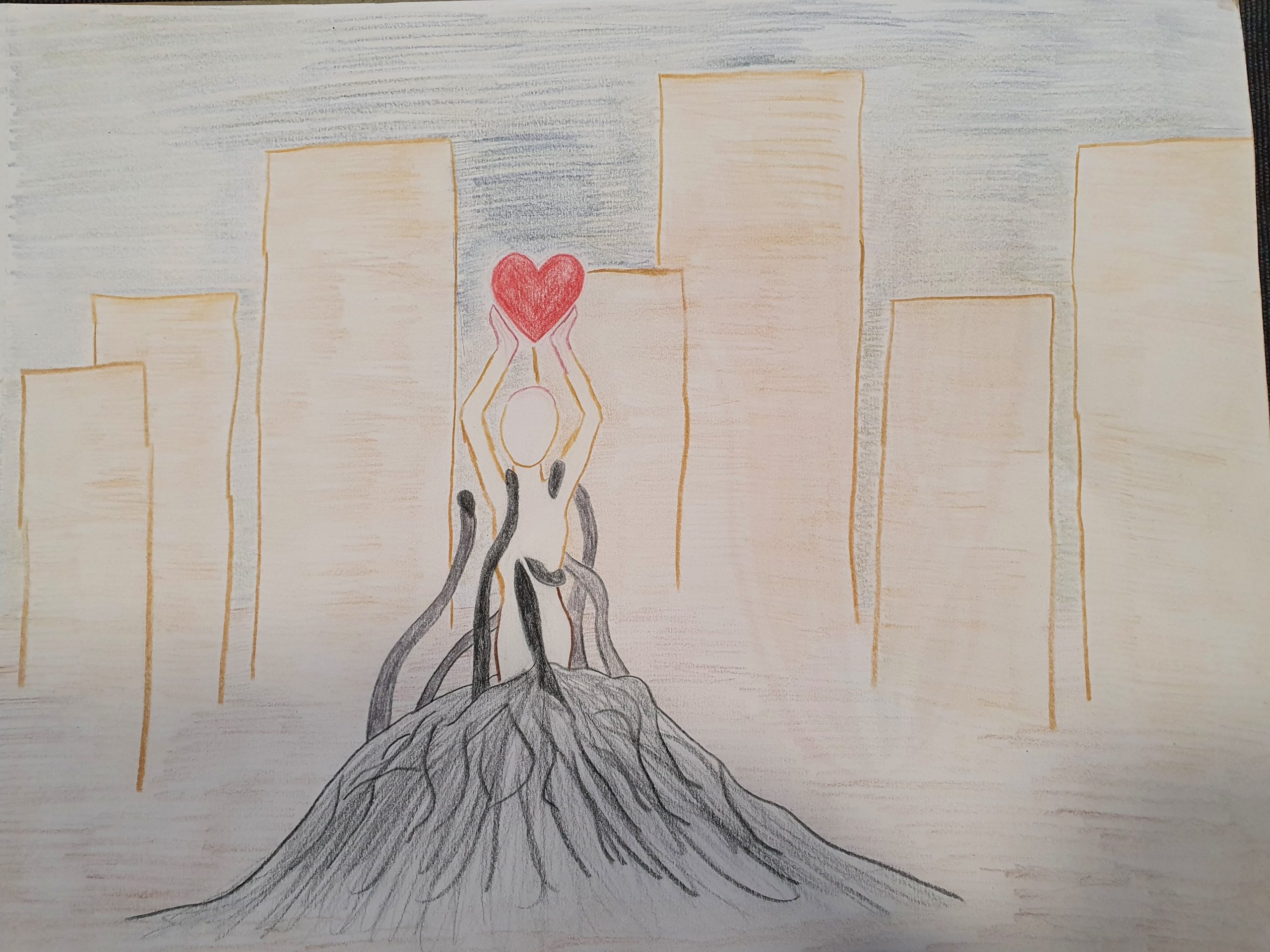
I found more of my people, people who accepted the authentic me, who let me be imperfect (as much as I don’t enjoy that for other childhood trauma reasons), who let me be vulnerable when I could shrug off the armour of the past. As pretty much nothing could be worse than my teenage years, I stood on my own and looked at those who would attempt to bully me, punish me, shame me, or make me feel unsafe and wonder why. I figured that office politics had two options, “you could play the game, or you could avoid it” but of course you can’t actually avoid it. So I did the next best thing, made myself indispensable and untouchable.
I’ve worked in so many toxic workplaces, and it is upsetting and stressful, but that’s because I’m watching bad things happen to good people. I haven’t had a perfect run through all of them, but generally people who would attempt to make my life difficult change their minds because I don’t react the way they expect. I can build enough psychological safety about myself, and buffer myself against workplaces that aren’t safe.
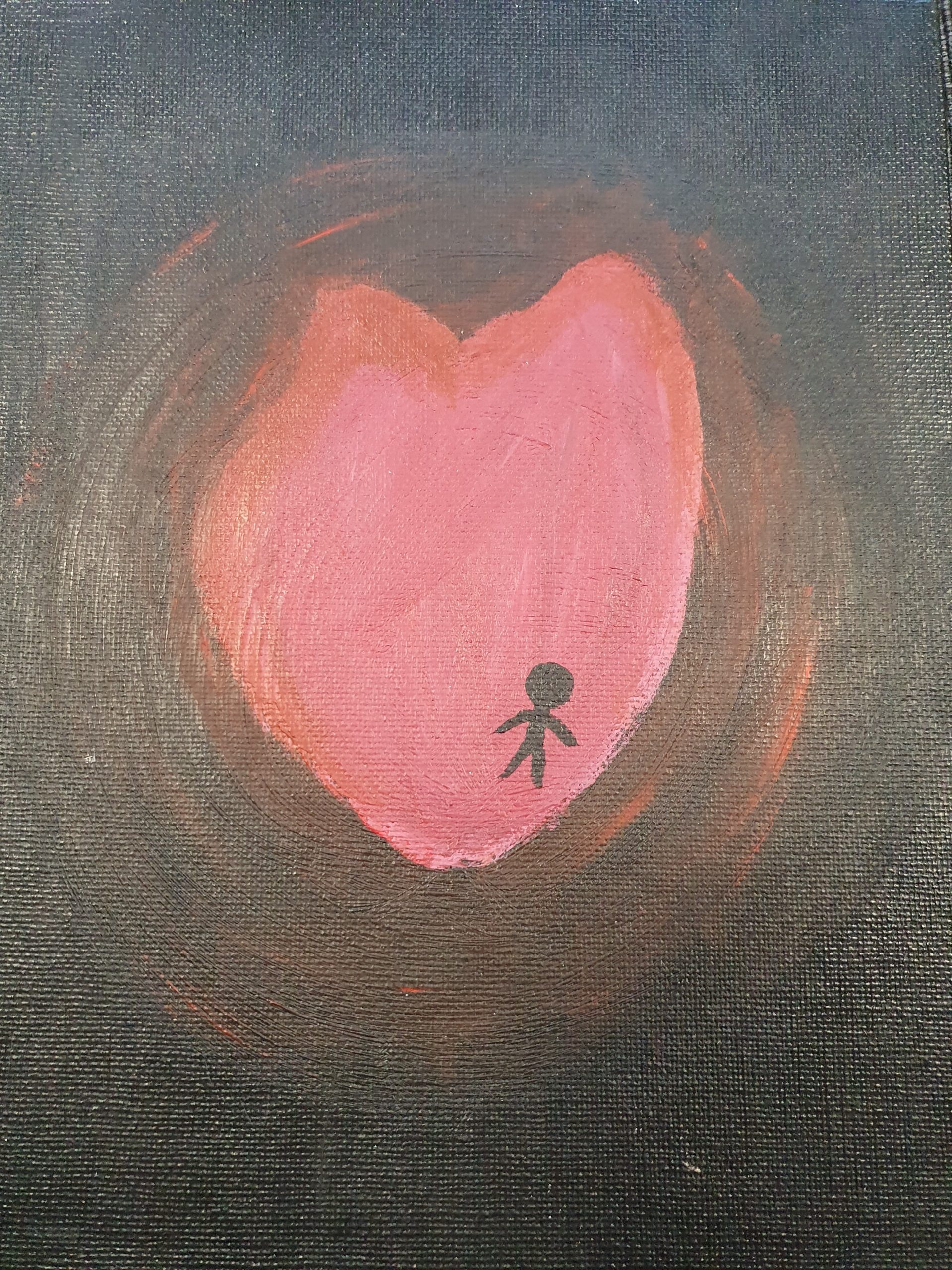
So that’s workplaces, but what about people who I’m friends with or who I move in the same community with or who I otherwise interact with? If it’s a person I am rarely going to interact with, then I ignore their difficultness and do my own thing. I don’t let them inside the bubble. If someone I am close to ends up being psychologically unsafe, whether it’s something temporary or long-term I distance myself from that person. I have ended friendships because people are unsafe for me, because I’ve felt attacked or shamed for some part of me.
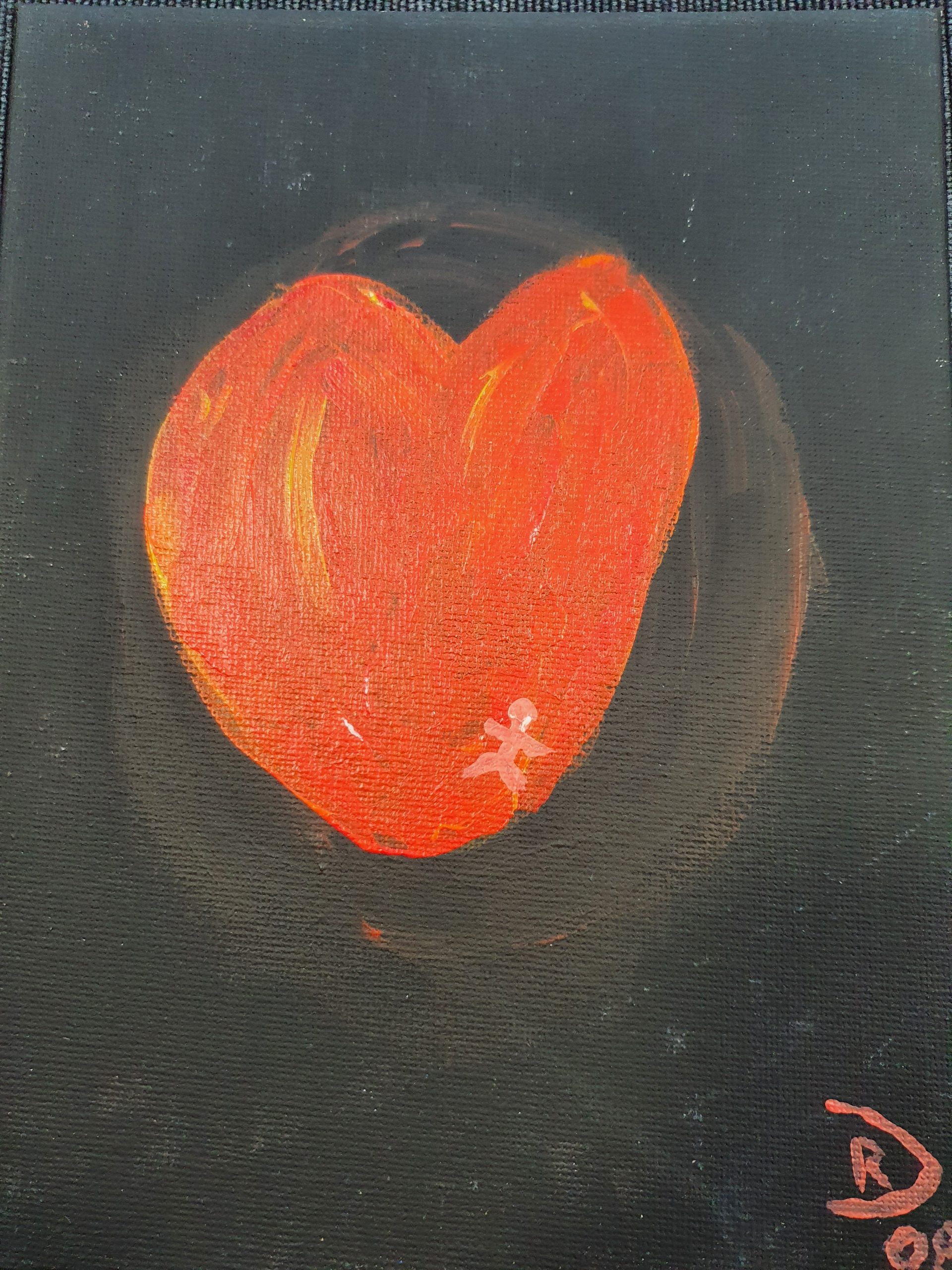
And this is also very gendered for me because of my childhood trauma. I am much more likely to feel at risk from people who were assigned female at birth than those who were assigned male. More girls and women have made me feel emotionally unsafe than men. And so I will walk away. It hurts, but my own psychological safety is more important to me than putting band-aid over band-aid on a relationship that is just going to keep hurting me.